-
Biotherapeutics
Regenerative product could provide new option for women with mesh exposure following pelvic reconstructive surgery

Research is advancing a regenerative solution for a quality of life-limiting complication of mesh-based surgical repairs for stress urinary incontinence and pelvic organ prolapse in women. While mesh-based surgical treatments are durable and provide symptom relief for a great number of patients, there is a risk of mesh complications following surgery, such as mesh exposure. In this situation, many patients require an additional surgery to revise their implant. Mayo Clinic research, supported by the Center for Regenerative Medicine, is testing a regenerative approach to restoring form and function without additional corrective surgery in the setting of vaginal mesh exposure.
Vaginal prolapse is a medical term for a condition that leads to bulging of the pelvic organs, such as the bladder, uterus or rectum. It happens when ligaments and muscles on the pelvic floor stretch and weaken, no longer providing adequate support. Those internal organs slip down, bulging through the vagina wall, causing prolapse. Alternatively, women can also experience accidental leakage of urine with activity or cough, laugh and sneeze. This is termed stress urinary incontinence. Often linked to child birth, obesity or aging, incontinence and prolapse affect many women.
Women with vaginal prolapse or urinary incontinence may choose to undergo placement of mesh if they have failed conservative therapies. Mesh is used in gynecology surgery to lift and support the pelvic organs, typically the bladder or uterus, relieving the pressure that caused the pelvic floor defect. However, like all surgery, there are potential risks. The mesh sometimes wears through the vaginal walls, causing vaginal discharge and possibly discomfort for women and their partners. Therein lies the dilemma: should there be another surgery to remove the mesh or would the patient prefer to live with the symptoms?
Mayo Clinic researchers are studying a new regenerative option, called purified exosome product (PEP) to treat a complication of the use of mesh in gynecologic surgery. Research, currently in animal models, is looking at whether PEP could promote regeneration of tissue that would grow over the mesh and restore the vaginal wall.
“While gynecological mesh is a viable option for many women, we wanted to create a non-surgical reparative option for our patients,” says John Occhino, M.D., clinician-scientist in gynecologic surgery with specialty training in urogynecology and pelvic reconstructive surgery. “We are studying the use of PEP to correct one of the most common side effects of mesh placement, the exposure of mesh through the vaginal wall after surgery.”
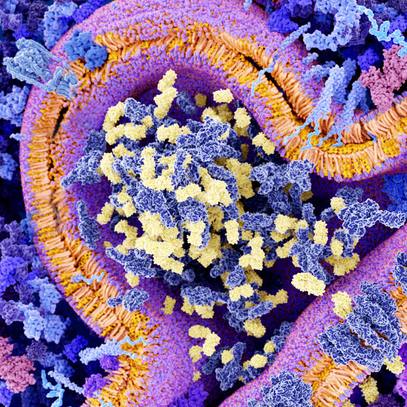
Exosomes are small membrane-bound vesicles secreted into the body’s cellular environment. Imagine bubbles carrying a signal that tell the body to regenerate and renew. For example, when the skin is scratched, exosomes are sent to repair the skin. By delivering a high dose of purified exomes, researchers can recruit numerous cells and pathways to help heal the tissue back to its original state.
“Our research injects an exosome gel into the vaginal tissues of a preclinical model of mesh exposure,” says Cassandra Kisby, M.D., female pelvic medicine and reconstructive surgery fellow. “Four weeks after treatment we saw the vaginal tissues had repaired and covered the prior mesh exposure.”
The regenerated tissues were physiologic, adds Dr. Kisby, meaning there were new blood vessels, the tissues had normal amounts of collagen, and there was minimal scaring.

While this research is currently only being done in animal models, Drs. Occhino, Kisby and team are working to develop a phase 1 clinical trial to test the safety of PEP in humans within the next year.
“This technology opens the door for numerous applications in gynecology, including birth injury and repair, urinary incontinence, and fistulas.” says Dr. Kisby. “Our goal is to create a women’s health regenerative medicine program to help expedite the research and translation of this technology into clinical practice.”
###
The Center for Regenerative Medicine recognizes Michael S. and Mary Sue Shannon for their generosity and support in advancing regenerative women’s health research.