Biotherapeutics

April 15, 2024
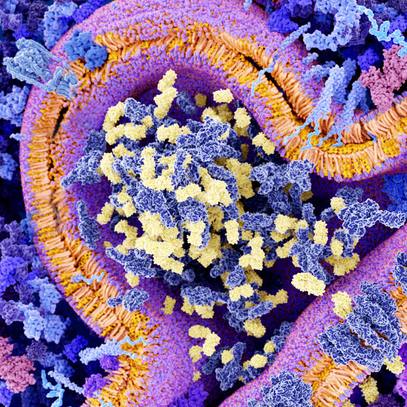
Gene editing, gene therapy and tissue engineering are emerging regenerative biotherapies that are on the cusp of transforming medical care. RegenBio Summit: Transforming Next-Gen Biotherapeutics[...]
April 2, 2024

March 12, 2024
January 31, 2024
January 17, 2024

November 30, 2023
Explore more topics
 Sign up
Sign up

Mayo Clinic Connect
An online patient support community