-
Biotherapeutics
The immune system and bone regeneration
Growing up as a student athlete in Cincinnati, Joe Panos had more than his fair share of visits to the orthopedist for sports injuries. The care he received for conditions ranging from pitcher's elbow to soccer sprains so impressed him that he vowed one day to be the physician instead of the patient.
Now Panos, an M.D./Ph.D. student in Mayo Clinic Alix School of Medicine, is hoping to become an orthopedic surgeon. As part of his education, he is conducting research to improve regenerative treatment for patients whose bones don't heal properly.
In early February, his research on how the immune system affects bone regeneration won the Orthoregeneration Award from the ON Foundation. That honor is given in collaboration with the Orthopaedic Research Society to a young investigator whose work advances orthopedic tissue regeneration.
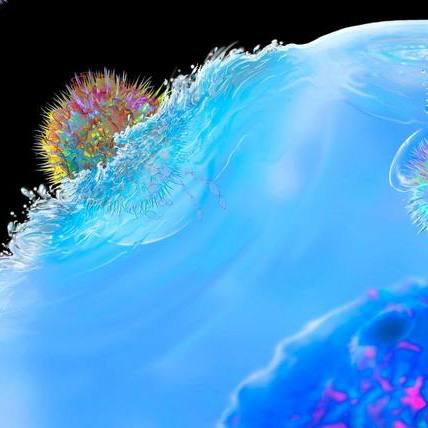
"When people have large fractures or lose part of a bone due to disease or injury, they don't heal very well. It's a really big clinical issue with very few effective treatments," says Panos. "Our research investigated immunomodulation, in which proteins activate or suppress the body's immune system and its ability to repair injured bones."
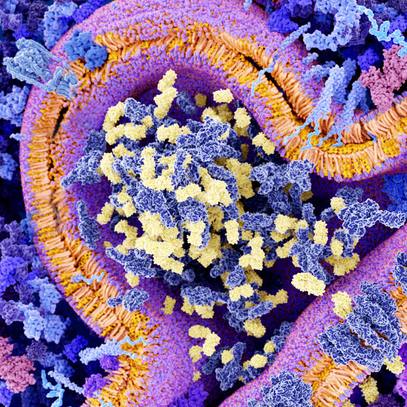
The field of regenerative medicine is seeking to shift the focus from fighting disease to rebuilding health, with an emphasis on repairing, replacing or restoring diseases cells, tissues or organs. Mayo Clinic's Center for Regenerative Medicine is at the forefront of this movement. The center supports Panos' research and education program as part of its objective of training the future workforce in regenerative medicine.
Less inflammation, more regeneration
Panos' research in the lab of his mentor, Christopher Evans, Ph.D., focused on bone morphogenic protein-2 (BMP-2), a growth factor that has been used to regenerate large fractures and bone loss. However, high doses are needed, which can be costly and cause life-threatening inflammation. The results are often only moderately effective.
"My abstract hypothesized that high doses of the growth factor BMP-2 and inflammation were related. We discovered BMP-2 released a blood-derived protein known as interleukin-1 that triggered the body's immune response," says Panos. "When interleukin-1 was blocked, we were able to lower the inflammation and regenerate large bone segments with 90% less BMP-2. The newly formed bone was just as strong and of higher quality than when higher doses were used."
Dr. Evans says this exciting finding could advance the practice by potentially making it less expensive and safer to apply the BMP-2 growth factor more widely to spur tissue regeneration more potently.
"It will help direct attention to the influence of inflammation in regenerative processes. This is something in which our lab is very much interested, not just in the context of bone healing, but also in the healing of cartilage, tendons and other tissues," says Dr. Evans. "Joe's discovery competed against submissions from researchers with far more experience. It is quite remarkable for a Mayo graduate student to win this Orthoregeneration Award."
Panos plans to use this research in the defense of his doctoral thesis this spring. After that, he will finish his final two years of medical school. His long-term vision is to advance orthopedic research in his career as a physician-scientist and apply regenerative medicine to treat patients like himself who have injuries from athletic or other trauma.
###