-
Biotherapeutics
Science Saturday: Identifying best candidates with avascular necrosis for regenerative alternative to hip replacement
A regenerative alternative to total hip replacement delayed the need for artificial implants by at least seven years for 35% of patients who had surgery to treat avascular necrosis. That condition occurs when blood flow to the hip joint known as the femoral head is constricted, causing bone cells to die. This Mayo Clinic research, which is published in Bone & Joint Open, also discovered that the size of the necrotic lesion and continued corticosteroid therapy affect the long-term viability of hip decompression surgery to relieve avascular necrosis of the hip.
Avascular necrosis is also a rare side effect of heavy steroid use as part of some chemotherapy treatment. Left untreated, tiny fractures from avascular necrosis worsen, and sometimes the joint collapses. Without hip decompression surgery, 90% of people with avascular necrosis need a total hip replacement.
"Saving a hip even for seven years is important because it delays the need of total hip replacement," says Rafael Sierra, M.D., a Mayo Clinic orthopedic surgeon and senior author of the study. "Many patients with avascular necrosis are younger than 50. By delaying or providing an alternative to total hip replacement, we may be able to prevent the need for a second or third hip replacement over the course of their lifetimes."
A great mystery of orthopedics
Avascular necrosis of the hip has been called one of the great mysteries of orthopedics. Once bone cells begin to die, nothing can stop the damage, unless it is caught early or there is intervention to try to restore the blood flow.
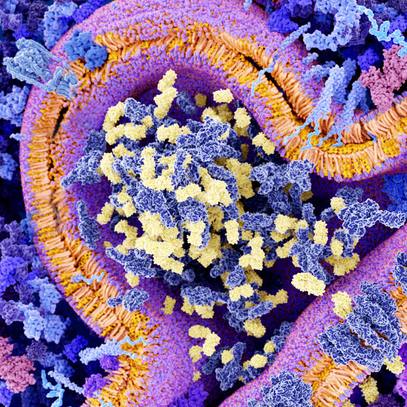
Mayo Clinic has been offering hip decompression surgery for over 15 years. This regenerative procedure taps the body's ability to heal decaying bone cells. A small hole is drilled in the outside of the bone to access the femoral head and release pressure with the hopes of improving blood flow to the damaged bone. A regenerative biotherapy is then injected to the hip joint to trigger healing. The biotherapy consists of the patient's mononuclear cells spun from bone marrow-derived mesenchymal (adult) stem cells. Mononuclear cells play a key role in cell repair.

Hip decompression surgery taps the body's ability to heal decaying bone cells. Mayo Clinic has offered this procedure for more than 15 years.
Regenerative medicine seeks to restore form and function by repairing, replacing or restoring diseased cells, tissues or organs. It's a fundamental shift in perspective from fighting disease to rebuilding health. Mayo Clinic's Center for Regenerative Medicine is at the forefront of this movement, and the center supports Dr. Sierra's research as part of its objective of bringing new cures to the practice.
The research
In a prospective study, Dr. Sierra and his team followed 22 patients with avascular hip necrosis who had been treated with hip decompression surgery. They were evaluated between five and seven years after surgery. Within seven years, 33% had progressed to total hip replacement for arthritis or worsening necrosis. However, the hip decompression surgery paused bone cell decay for two-thirds, and they did not require additional surgery.
The research team documented that use of corticosteroids and the size of the bone lesion prior to surgery were risk factors that expedited the need for a total hip replacement.
"We found that patients who were on steroids had a four times higher risk of progression than those who were not taking steroids at the time of surgery," says Dr. Sierra. "Patients who had larger areas of joint decay in the femoral head had a survivorship of about 40% at seven years, compared to about 72% at seven years for those who had smaller lesions. If you take the group as a whole, approximately 10% of patients per year who have had hip decompression surgery will need to go on to have a total hip replacement."
The research identifies ideal candidates for hip decompression surgery as those in earlier stages of avascular necrosis and those who are not on corticosteroid therapy. Dr. Sierra would still recommend the surgery for all patients, including those with higher risk factors.
"Hip decompression surgery is such a small procedure with such a quick recovery that there's really no downside. It's not like if we do hip decompression, we're not going to be able to do a total hip," says Dr. Sierra. "They can have this and delay hip replacement for a couple of years, or maybe they'll be within that 70% that make it seven years before they need a total hip replacement. And if that's the case, then that's a huge benefit to them."
Dr. Sierra has performed as many as 300 hip decompression surgeries, allowing patients to delay or even prevent a total hip replacement surgery. While Dr. Sierra also performs hip replacements when necessary, he says it's in the patient's best interest to delay or avoid that surgery.
"With each passing year, we learn more and refine total hip replacement surgery. Who knows what types of advancements there'll be for patients who can wait two, three or more years for this surgery," adds Dr. Sierra.
###