-
Biotherapeutics
The dawning of regenerative neurosurgery
Regenerative neurosurgery is poised to transform care of neurological disorders that previously had little hope for improvement, according to a Mayo Clinic review published in The BMJ. Healing diseases of the central nervous system remains a highly coveted but formidable challenge, Terry Burns, M.D., Ph.D., a neurosurgeon scientist at Mayo Clinic, writes in a synopsis of regenerative medicine research. His synopsis spans neurosurgical efforts to treat neurodegenerative diseases, stroke and spinal cord injury.
After decades of developing and refining new regenerative tools and methodologies, Dr. Burns theorizes that neurosurgery is positioned to advance new therapies that unleash the body's ability to repair diseased tissues and cells.
"Regenerative neurosurgery provides access to the central nervous system or its surrounding structures to preserve or restore neurological function," says Dr. Burns. "Strategic multidisciplinary efforts will be critical to harness complementary technologies and maximize mechanistic feedback, accelerating iterative progress toward cures for neurological diseases."
Expanding the regenerative medicine toolkit
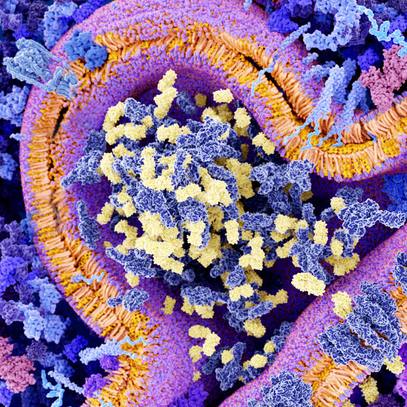
The human neurological system is a complex web of more than 100 billion neurons connected by over a quadrillion nerve junctions known as synapses. For centuries, medical science considered nerve patterns fixed and incapable of adapting, changing or healing. As a result, the prognosis has been poor for restoring diseased neurons found in conditions such as Parkinson's disease; Lou Gehrig's disease, or amyotrophic lateral sclerosis (ALS); and multiple sclerosis.
The emerging field of regenerative medicine, with its focus on repairing, replacing or restoring damaged cells and tissues, is galvanizing clinical innovation. The discovery of embryonic stem cells that can transform into different types of cells, neural stem cells found in the nervous system, and induced pluripotent stem cells that can be reprogrammed to become different types of replacement cells help expand the regenerative toolkit for repairing central nervous system disorders.
"The rise of stem cell technologies over the past 25 years has energized clinical hopes of regenerative cell therapies," writes Dr. Burns. "Neurosurgery offers an avenue for directed cell implantation into the sites of disease within the brain and spinal cord."
Early clinical trials at Mayo Clinic are probing whether mesenchymal stem cells derived from adipose, or fat, tissue could provide growth factors and anti-inflammatory properties to protect nerve cells from dying, thereby halting disease progression. Mesenchymal stem cells are adult stem cells that have been well-studied. Results of a phase 1 clinical trial at Mayo Clinic discovered that 30% of ALS patients stabilized after mesenchymal stem cell intervention. Mayo Clinic also is studying the effects of stem cell therapy on spinal cord injury. A case study of the first person enrolled in a phase 1 clinical trial found the patient regained some function after mesenchymal stem cell lumbar injections and physical and occupational therapy.
"These are some promising examples of patients who have regained function or seen their neurodegenerative disease stabilize after participating in neurosurgical trials of regenerative therapies," says Dr. Burns. "However, this remains a relatively young field and much more work is needed to refine strategies and ensure the most appropriate patients are treated with the most effective therapies at the right time. Because the human brain is so unique, there are no ideal animal models for most neurological diseases, and no substitute for pioneering studies in human patients to push things forward."
Dr. Burns says it's imperative that the most advanced technologies, including artificial intelligence, machine learning and biomarkers, are used to help identify which patients are most likely to benefit from regenerative therapies in clinical trials.
"Carefully designed studies are needed to ensure new therapies are safe. It's important to figure out what is going to create an environment that helps regenerative therapy work best," says Dr. Burns. "A lot of critical work still lies ahead to safely and effectively bring the promise of regenerative therapies into clinical practice for neurological diseases."
Given a historically poor ability to accurately predict or sensitively measure small changes in patient outcomes for most diseases, most neurosurgical trials to date have been focused on demonstrating safety. As a result, progress has been slow. However, the pace of clinical trials is increasing, and some encouraging advancements are being reported in areas such as gene therapies for rare genetic conditions.
"It is exciting that we now have a robust and growing inventory of regenerative neurosurgical tools from cell and gene therapies to devices and infusions. As biomarker feedback and machine learning tools come online to better individualize therapies and more quickly recognize patterns of benefit, progress will accelerate further. I think the next decade is going to be very exciting for regenerative therapies, finally demonstrating their value to clinical practice," Dr. Burns says.
###