-
Biotherapeutics
Could regenerative medicine hold a key to understanding Alzheimer’s disease?

September is World Alzheimer’s Month, a time to raise awareness of research to unlock scientific mysteries around a disease that robs people of their memory, independence and ultimately their ability to think and reason. Focused on disease causes and cures, the Center for Regenerative Medicine is driving innovation as a collaborative partner in Mayo Clinic’s robust research to increase understanding and to slow or stop the progression of a neurological disorder for which there are no approved treatments to alter the course of disease.
Alzheimer’s disease affects 1 of every 10 people over the age of 65, or more than 5 million Americans, according to the Alzheimer’s Association. That number is expected to grow exponentially in coming years amid a rapidly increasing older adult population. Working collaboratively with Mayo Clinic’s Alzheimer ’s Disease Research Center, Center for Regenerative Medicine researchers are using the latest cellular technology along with regenerative approaches to better understand disease progression and possible regenerative treatments.
A regenerative approach to Alzheimer’s disease
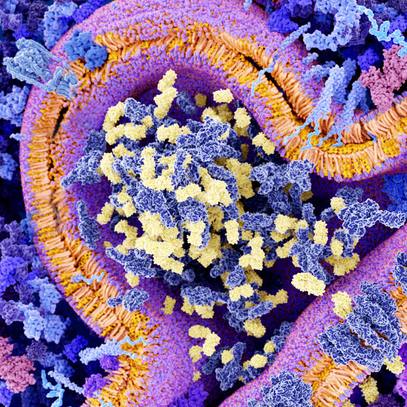
Genetic, lifestyle and environmental factors are believed to play a role in Alzheimer’s disease. However, the biggest risk factor is advanced age. Neurological and memory decline — the hallmark of Alzheimer’s disease — is related mainly to two different types of proteins. The accumulation of amyloid-beta plaque interferes with neurons, resulting in a decline of brain cognition. Abnormal amounts of the protein tau causes tangles that become toxic and eventually kill the neurons in the brain. It’s a complex disease, however, and at the time of autopsy, many different abnormal proteins may be found in the brain.
Preclinical neuroscience research within the Center for Regenerative Medicine in Florida has focused on genetic risk factors linked to the apolipoprotein E (APOE) gene. The APOE gene has different versions called variants that impact the risk of Alzheimer’s disease. Laboratory studies that model the risk variant, APOE ε4, in mice discovered an increased degenerative effect on the brain, compared to the lower risk variant APOE ε3.

“We found if we change this APOE genotype in the peripheral blood, it can affect brain cognition and amyloid-beta pathology. The ε4 genotype would impair brain cognition, but a switch to ε3 made the brain function better,” says Guojun Bu, Ph.D., chair of Neuroscience in Florida and associate director of Center for Regenerative Medicine in Florida.
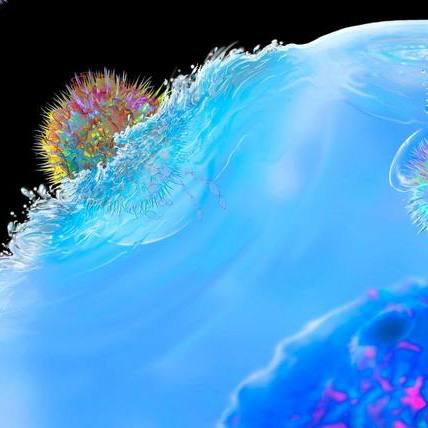
This discovery at Mayo Clinic in Florida has laid the foundation for phase I safety studies in humans. Researchers in Florida want to apply their genetic findings to the study of potential healing qualities of blood plasma. In particular, they want to answer the question of whether plasma from young donors without Alzheimer’s genetic risk factors would have regenerative effects on individuals with the APOE ε4 risk variant who are in the early stages of Alzheimer’s. Young donors would be people 30 years old or younger.
“We know from outside research that young plasma in general has a rejuvenating, regenerating ability in age-related conditions and aging in general,” says Dr. Bu. “Testing whether an injection or even a complete exchange of young plasma might have therapeutic effects in early stage Alzheimer’s patients with the APOE ε4 gene variant is very intriguing.”
Currently, little is known about restorative healing in the aging brain. Traditionally, the brain has not shown to be prone to regeneration as it ages, according to Melissa Murray, Ph.D., a neurosciences researcher at Mayo Clinic in Florida.

“Our knowledge gained from neurodevelopmental studies suggests that specific signals are released when our brains are more plastic and capable of growth. Some focus has been paid to identifying if those signals could be turned on to facilitate regeneration,” says Dr. Murray. “There is still so much unknown, but neuronal regeneration should not be ruled out in this modern era of technological advances in stem cell therapy or with the potential for plasma donors.”
Creating mini brains to study Alzheimer’s disease
One of the hurdles to overcome in Alzheimer’s disease research is the absence of a model in which amyloid-beta plaques and tau tangles can be studied together. Animal models, which have been studied for years, don’t always reflect disease progression within the human brain.
“The mouse brain is quite different from the human brain anatomically and at the molecular level. Animal findings don’t always translate to humans,” says Dr. Bu.
The brain bank in Florida, which provides more than 5,000 post-mortem specimens, including 3,000 from Alzheimer’s patients, has been a key resource in advancing research into the cause and progression of neurodegeneration. The brain bank helps with defining how disease-associated pathologies correlate with gene expression, biomarkers and clinical information.
Now, researchers are taking their research a step further by growing human mini brains in a laboratory dish. Using induced pluripotent stem cells (iPSC) reprogrammed from skin fibroblasts or peripheral mononuclear cells, researchers are able to grow 3- to 4-millimeter living organoids resembling the structure of human brains including layers of neurons and ventricles. IPSCs are stem cells that are reprogrammed in labs but are similar to embryonic stem cells. They are now routinely generated in the Center for Regenerative Medicine infrastructural facilities such as Regenerative Medicine Biotrust and Neuroregeneration Lab. An embryonic cell can be redirected to become a brain cell for the purposes of creating a disease-in-a-dish for research.
“These living mini brains come from cells of individuals with Alzheimer’s disease,” says Dr. Bu. “With this model system, we can see more precisely what is happening within the Alzheimer’s brain and the effects of APOE ε4 gene variant. That helps us to study the cause and progression of the disease. We hope this brain-in-a-dish model will lead to an understanding of the Alzheimer’s pathology and how to target treatments that can slow or stop progression of the disease.”
When a therapy is someday identified, an individualized approach will be needed to successfully prevent or delay the onset of symptoms, Dr. Murray adds.
“Treatment approaches are different for young onset Alzheimer’s disease, which develops in people under the age of 65, and late onset, which affects those over 65,” says Dr. Murray. “This is due to differences in where abnormal proteins accumulate and how often co-existing pathologies occur in the aging brain.”
Dr. Bu envisions future therapies that take a multi-pronged approach to treating amyloid-beta plaque, tau tangles and loss of neurons. Many phase I, II and III clinical trials are underway in the quest to move the latest laboratory discoveries into daily standard of care. Dr. Bu says realistically, it could take anywhere from five to 20 years for a drug to obtain Food and Drug Administration approval in the United States and bring new therapeutic options to Alzheimer’s patients.
###