-
Biotherapeutics
Science Saturday: Seeking a regenerative therapy for chronic dry mouth
Mayo Clinic researchers are seeking a regenerative therapy for a vexing problem, particularly among cancer patients. How can medical providers treat a condition in which the mouth is so parched that it has an incessant feeling of a cotton lining? Xerostomia, also known as chronic dry mouth, is an agonizing side effect of injury to the salivary glands. While it is most common after radiation treatment for head and neck cancer, it also afflicts people with diabetes, stroke, Alzheimer’s disease and HIV/AIDS.

“Dry mouth is something that when you have a life threatening illness, at first may not seem like a big deal. However, this condition can extend long after radiation treatments are complete. It’s probably the top concern I have from head and neck cancer patients. Unfortunately, there aren’t many therapeutics available commercially for these patients,” says Jeffrey Janus, M.D., an Ear, Nose and Throat specialist at Mayo Clinic in Florida.
Currently there is only supportive care — no cure — for the decrease in saliva that comes from xerostomia. Besides being uncomfortable, chronic dry mouth can lead to difficulties with chewing, tasting, speaking and swallowing. It can also cause tooth decay.
Mayo Clinic Center for Regenerative Medicine, Department of Laboratory Medicine and Pathology and Department of Otolaryngology are collaborating on ways to address the unmet needs of these patients.
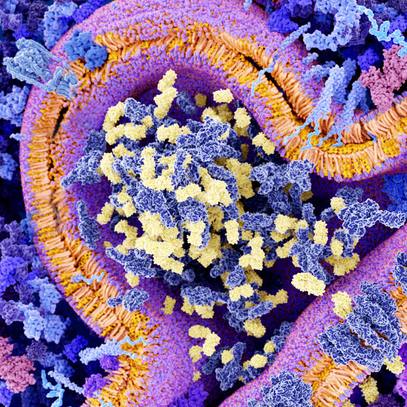
The question investigators are seeking to answer is whether the body’s healing abilities could be unleashed to restore natural lubrication of salivary glands. The research will focus on the regenerative abilities of epithelial cells found within many glands in the body, including salivary, mammary and prostate glands. They hope to discover whether epithelial cells could be tapped to regenerate salivary gland tissue to produce natural saliva.
Building on existing research
Previous studies showing epithelial cells purified from mammary glands could regenerate functionally-intact mammary glands piqued the interest of the research team. Could the same concept be applied to heal and restore saliva in salivary glands? Their research will build on this existing body of knowledge.

“In many ways salivary glands resemble mammary glands. As early as 2006, it was shown that a single transplantable mammary cell could regenerate highly complex lactational structure. That was the genesis of the concept that glands represent epithelial stem cells and that we might be able to harness these rare cells for treatment of dry mouth,” says Nagarajan Kannan, Ph.D., a scientist with the Department of Laboratory Medicine and Pathology and head of the Stem Cell and Cancer Biology Lab at Mayo Clinic.
To validate this theory, the team has identified a few hurdles to overcome that could stall the research.
First, they need robust human tissue samples to test their theory. They’ve planned to establish a biobank of the three different types of human salivary glands with samples from consenting men and women. Second, they are developing robust methods to isolate and study epithelial cells from salivary glands. Third, they need a model in which to investigate whether those cells could regenerate human salivary tissue. To address this issue, they will study epithelial cells in immune-deficient mice that have been biologically engineered to mimic injured human salivary glands.
“Using this model, we can now start testing how the salivary cells permanently engraft and regenerate into salivary structure and restore saliva. Our model measures how saliva production drops and holds at a decreased level. It is the best model available for studying how human salivary samples perform over time,” says Dr. Kannan.
No specific date has been set for advancing this concept into human clinical trials. However, Dr. Kannan and Dr. Janus are hoping the preclinical studies will lay the foundation for early safety studies within the next year or two.
“I’m hopeful that if we can show this is safe and effective, we can immediately transition into using this regenerative procedure using silo endoscopy, which is like endoscopy of the salivary glands, to implant these cells in early clinical trials,” says Dr. Janus.
Accelerating the findings toward clinical practice is a priority. The team will not only work across departments at Mayo Clinic, but will also collaborate with experts outside of Mayo Clinic to move the research forward as quickly as possible.
###